Cloud
Application
Hosting

Contact
Us

Cloud
Application
Hosting

Application
Development

Mobile
Applications

Data
Interfaces

Enterprise Data
Visualization &
Analysis

Incident
Management
Risk
Assessment

Risk
Management
Suite
The Zoldak Group


Process Risk
Management

Workers
Compensation


Risk Management Technologies
hhhhhhhhhhhhhhhhhhhhhhhhhhhh hhhhhhhhhhhhhhhhhhh hhhhhhhhhhhhhhhhhhhhh
hhhhhhhhhhhhhhhhhhhhhhhhhhh hhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhhh
yyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyyy
yyyyyyyyyyyyyyyy yyyyyyy
RMS Workers’ Compensation Claim Management Module



Developed by ZGi
© 2014 The Zoldak Group, Inc.

The ZGi Risk Management Suite Compensation Module (CMM) supports all claim
management functions in support of Federal Employee Compensation Act
program requirements from electronic claim submission though return to work.
Claim Management, Analysis, POWER: The CMM supports both the claim
management process and provides analytical tools and thereby directly supports
the Protecting Our Workers and Ensuring Re-employment (POWER) Initiative.
When used with the ZGi Incident Analysis Module for managing occupational
injuries and illness, it provides a totally integrated claims management and risk-
based occupational safety and health system which leverages and data from the
safety and claims management process. This technique has been proven in
reducing injury, illness, and compensation rates by identifying opportunities and
assessing the results of agency risk-reduction initiatives.
Record Access Control Profiles: The RMS Security Module maintains profiles allowing users to access
records by agency organization level. Profiles also provide for individuals to access safety-only, claim-only,
or both. Data from each is leveraged for efficiency and consistency.
The CMM consists of the following sub-modules:
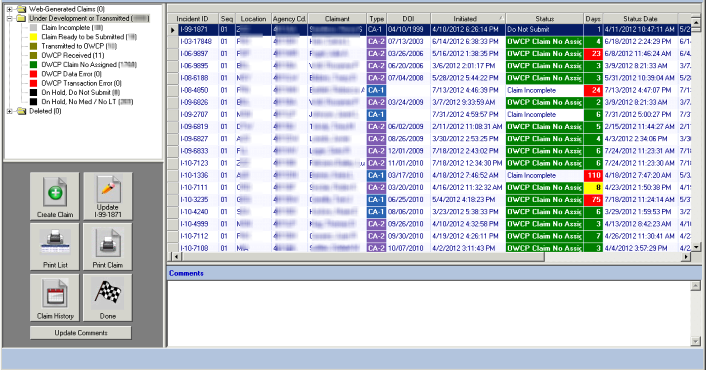
Claim Wizard: Used by Workers' Compensation Professionals (WCPs) to initiate and submit claims to the
Department of Labor's Office of Workers' Compensation Programs (OWCP). It provides a step-by-step
approach to completing a claim. Related employee data and agency information are automatically
populated to save time and improve efficiency and accuracy. The Claim wizard tracks the claim from
initiation, through OWCP validation and claim number assignment. The Claim Wizard is proven and has
been successfully used to submit thousands of claims electronically to the OWCP.
CMM Web Module: This optional CMM component provides employees with the ability initiate a CA-1 or
CA-2 claim online. Automatic data population and validation reduce the chance for errors and speeds up
the process. When the employee has completed Part A, an electronic notification is sent to the
supervisor who completes Part B. Finally, the claim is imported, reviewed and submitted to OWCP via the
Claim Wizard by authorized WCPs.
Claim Management Segments: Claim management is accomplished via secure record segments that
maintain a complete claim history beginning at submission. There are two types of segments, those
updated electronically from OWCP or those maintained during the course of claim management by WCPs.
The former include: Claim Status, Reported Conditions, Medical Costs, and Wage Compensation Costs.
Note all ICD9, procedure, and NDC codes are translated. Local claim management segments include:
Controversion, Challenge, Limited Duty, Compensation, Third Party Action, Privacy Disclosure Tracking,
and Leave Tracking including: Request, Medical Limitations, Job Offer, Work Schedule, and Suitability.
Claim Media: External PDF, Excel, Word or picture files are stored separately from similar media used to
document the incident for privacy. This restricts viewing of Privacy Act information to WCP and other
authorized individuals.
Interfaces: A variety of system interfaces maintain agency reference data (e.g., human capital, payroll,
organization, etc.) as well as support the submission of claims to OWCP and receiving status updates (e.g.,
NCMF for claim status, BPS for detail medical costs, ACPS for wage compensation costs, and Chargeback
data).
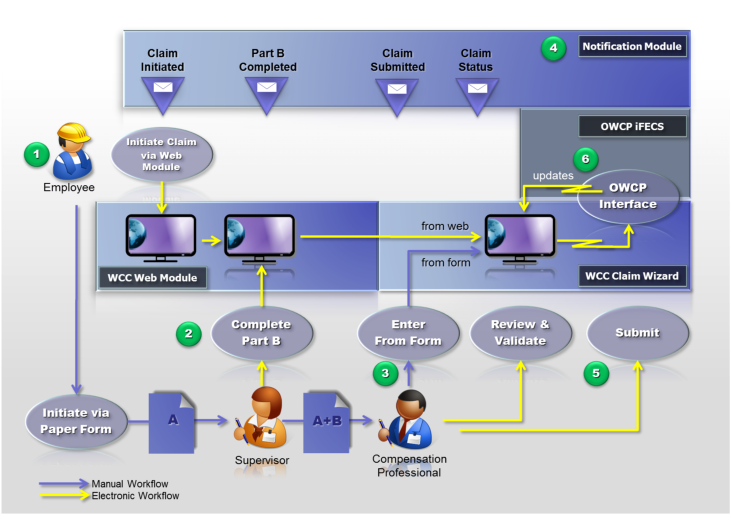
Claim Management Workflow: The CMM components are configurable to suit specific agency
requirements. This efficient, collaborative workflow is summarized in the figure below. It results in time
savings, sustaining a collaborative claim management environment, and establishes an enterprise,
analytical database that supports reducing total and lost time case rates, increasing the timeliness of
filing, reducing lost production days, wage losses, and speeding up return to work. This directly and
uniquely supports the POWER Initiative.
1.
Employees initiate a claim via the Web Module or paper form.
2.
Supervisors complete the paper Part B or online.
3.
Workers' Compensation Professionals review the paper form or the electronic record, validate it
and submit it to OWCP if there is lost time or medical costs. Others are maintained locally unless
or until lost time or medical costs are experienced by the employee.
4.
Electronic notifications ensure that all stakeholders are in the loop.
5.
Claims are submitted electronically
6.
After the claim has been submitted the local claim is updated with status, adjudication, cost, etc.
data automatically. This information is used to manage the claim and for overall reporting,
analysis, rate calculations, etc.




Claim Submission
Claim Status
OWCP Interfaces
Reported Conditions
Costs
Controversion
Challenge
Limited Duty
Leave Tracking
Third Party Action
Privacy Disclosure
Analysis